2025 Blogs & Vlogs – Employment Opportunities and Challenges for People Living with Adrenal Insufficiency or Pituitary Disorders
We are happy to launch the new 2025 WAPO Blogs and Vlogs series which, this year, will feature a video interview and an accompanying blog article that highlights key takeaways and provides extra resources to learn more about the topic covered.
For our first installment we are honored to feature Johan G. Beun, ambassador of AdrenalNet (BijnierNET in Dutch). Johan shares his expertise on the topic of employment and the challenges faced by people living with adrenal insufficiency or a pituitary disorder, following a Dutch multi-stakeholder project. This article provides a summary of the Vlog interview that you can find on the WAPO website’s Library and YouTube channel.

What is AdrenalNet and Adrenals.eu?
AdrenalNet (BijnierNET) was founded in 2015 in the Netherlands by the six University Medical Centers, two patient organizations and the Dutch Society of Endocrinology (NVE). It was created to address the lack of information available about adrenal conditions in the Netherlands. In the Netherlands, there are approximately 12,000 to 14,000 people using hydrocortisone, most of whom are adrenal patients. AdrenalNet recognized that creating a single, comprehensive, and high-quality information website would be more effective than having individual hospitals all develop their own resources. While initially focused on the Netherlands, AdrenalNet received enquiries from other countries, particularly in Scandinavia, where they already collaborated closely with the Danish Adrenal patient organization (Addison Foreningen Danmark). Additional enquiries have come from Germany, Belgium, France, and more distant locations such as Canada, Australia, New Zealand, Thailand, and Singapore. Nowadays, AdrenalNet (www.BijnierNET.nl ) serves at least 15,000 unique visitors monthly and,adrenals.eu (the international website) serves 7,500 unique visitors monthly.
What are the most common challenges that people with adrenal insufficiency or a pituitary disorder face in terms of employment?
Johan acknowledged the complexity and seriousness of the challenges faced by patients with adrenal insufficiency or pituitary disorders when it comes to employment. He pointed out the prevalence of “pseudo-privacy rules” and the tendency for professionals to work in silos. For example, many doctors transition into insurance roles and there are endocrinologists who avoid communicating with insurance experts, which results in patients being left in the dark about the overall process.
He emphasized that this lack of coordination impacts various professionals, from general practitioners and occupational health physicians to internal medicine specialists. Although all of these professionals have good intentions, the reality is that the system often fails the patients, who are left without the support they need. This lack of patient-centered collaboration leads to suboptimal diagnostic processes, delayed diagnoses, and inadequate treatment. Women also face additional challenges due to gender bias, as they are often dismissed with explanations like, “It’s your hormones” or “Are you menopausal?” causing delays in receiving proper care.
In the Netherlands, another issue is the 24-month deadline for making a diagnosis and establishing a treatment plan in order to qualify for rehabilitation programs and reinsurance schemes. Unfortunately, this timeframe is often too short, creating both physical and financial problems for patients.
Johan also brought up the psychological issues that frequently go unaddressed. Many people hesitate to seek help for the mental health effects of their condition. Johan argued that a more integrated approach is needed that combines employment, healthcare, and mental health support. He stressed that these three elements must worktogether to ensure that the patient’s physical, emotional, and professional needs are met.
Can you briefly talk to us about the Dutch “Participation in Employment” project that you were involved in and its main findings/results?
This initiative began as an exploratory research project aimed at understanding how healthcare and work participation intersect, and where challenges occur.
Despite operating with a very limited budget, it gave rise to significant results, largely due to the enthusiasm and collaboration of its participants.The project brought together a diverse group of professionals and stakeholders including labor experts, insurance physicians, patients, patient advocates, endocrinologists, rehabilitation specialists, physiotherapists, and nurses. Their shared insights revealed the importance of collaboration and knowledge exchange. Johan described it as being like a painting, with all of the experts contributing a single color, but the final piece of art being a beautiful mix of all these colors.

For individuals with rare conditions like adrenal insufficiency, additional hurdles such as privacy constraints, knowledge gaps, and delayed diagnoses only amplify the challenges. This underscores the urgent need for more shared knowledge and collaboration across disciplines to better support these patients in both healthcare and work settings.
Johan shared how diagnosis times for adrenal diseases have significantly improved over the years. When he first started working in healthcare, it could take up to 25 years for patients to receive a diagnosis. Today, the average time ranges between one and 2.5 years, which, although better, is still too long. He emphasized the need for expertise to be shared and for healthcare information to be neutral and accessible. It is this thinking that inspired the creation of the following factsheets during the course of the project:
Adrenal Insufficiency FACTSHEET (soon to be available – add link)
Johan mentioned the positive impact these factsheets have already had. They have allowed all doctors, insurance experts, labor experts, and rehabilitation experts to truly understand the essence of the various diseases. Johan explained that the project removed the usual barriers, allowing the group to create the building blocks for these factsheets collaboratively. For Johan, the creation of reliable, neutral, and comprehensive healthcare information is essential for improving the lives of adrenal and pituitary patients.
How can healthcare providers play a role in reducing work disability/preventing unemployment?
Johan explained that the question of work and illness is complex because employers usually hire employees to work for them in exchange for money. However, work is not just about earning money; it is an integral part of a person’s life. Many people derive pleasure from their work, gain their social connections through work, and truly take pride in what they do.
He emphasized that while someone with adrenal insufficiency or a pituitary disorder may not be the “perfect employee” in traditional terms, they still have a lot of valuable capabilities left to offer. Rather than focusing on what a person cannot do, we should focus on what they can still contribute to both society and to their employer.
He stressed the need for flexibility in the workplace, rejecting the thought of “either you’re good enough to work or you’re not.” He pointed out that most people, even those facing a rare disease, are capable of working in some capacity.
Unfortunately, too often, patients are caught in a cycle where healthcare providers and employers focus on insurance and financial aspects, rather than considering the long-term well-being of the patient. For Johan, the goal should be for healthcare providers to prioritize “the health and wealth of the patient in the long run”, ensuring they can still participate in employment while properly managing their condition.

What practical actions can employers do to better support employees living with one of these conditions?
Johan shared his perspective as someone who has experienced different roles as an employer, employee, and now, as a “pensionado in training.” He admitted that he has not yet fully embraced retirement as he loves his work.
He highlighted the need to better inform employers about how they can support employees with adrenal insufficiency or a pituitary disorder. By providing flexibility and making adjustments (such as allowing employees to work from home, if appropriate) patients are encouraged to stay connected to their work and continue to contribute. In his opinion, having employment, even in a reduced capacity, is essential for the employee’s sense of purpose and well-being.
Johan also touched on the challenges within the Dutch system, where discussions are often centered on income, health insurance, and employer’s insurance. He argued that the focus should shift from purely financial considerations to the employee’s overall happiness and well-being. He suggested that employers should receive regular updates on the health and progress of their employees, ensuring that decisions are made with the patient’s best interests in mind rather than focusing solely on financial discussions.
What should people newly diagnosed with one of these conditions consider in regards to their career and maintaining a healthy work-life balance?
Johan suggested 5 items which need to be considered when trying to address this question:
1) Delayed diagnoses are common when it comes to pituitary and adrenal conditions. If you fear that you are in a hospital where the right expertise is lacking, you must try to seek care at hospitals with expertisein these conditions so that you can have a timely diagnosis. In the Netherlands, there are approximately 70 to 80 hospitals and only 10-30% of them have expert endocrinologists specializing in these conditions. Accept that there may not be a hospital in your town with expertise on your disease and that you may need to discuss options on how to access expert care.
2) Talk to your general practitioner and your endocrinologist, and share your concerns when it comes to treatment. Ask them about their experiences, especially when it comes to pituitary surgery. According to Johan, such surgeries require “super experts” and should only be performed in a few specialized centers. In the Netherlands, with a population of roughly 18 million people, he suggested that only two or three hospitals should handle these pituitary operations. Similarly, for adrenal removal, there are about 400-450 operations per year in the Netherlands, and they should be centralized to five or six hospitals to ensure high-quality care. Be open to being referred to a specialized center, as this is critical for achieving the best outcomes.
3) Do not be afraid to share your doubts and concerns with your doctor about your employer. Similarly, do not be afraid to share your doubts with your employer. Everyone benefits if you can continue your work and it is better to continue to work at 50% capacity for the rest of your life than to sit at home because you could not prove that you were able to work at 100%. Any work capacity is valuable to you, your employer, society, and your family. He stressed that “sitting at home and doing nothing is absolutely a disaster. Work is an essential element of well being”.
4) Please do not think that your condition is only a physical medical problem. He recommends reaching out for help, whether this help is from the social worker at your workplace or the psychologist at the hospital. You may need to see a psychiatrist, as your life has dramatically changed and will never be the same.
He emphasized that acceptance is the key to navigating life with a chronic condition and that the sooner and better you accept your new reality, the happier you will be. Embracing this mindset not only improves personal well-being but also enables individuals to be more present and engaged in their work, relationships, and family life as “no matter what you think, your family still relies on you.”
5) Manage your expectations and accept that life has changed. Johan reflected on his own journey. After having earned his first academic master’s degree at 21 he felt on top of the world. However life handed him some moments of “bad luck” and despite these events, he has managed to persevere and stay optimistic thanks to the help of his wife, family, and psychiatrist. The key, he emphasized, is to manage expectations. “Don’t expect that life is the same tomorrow as it was yesterday”.

What advocacy efforts are still needed in this area?
According to Johan, there is unfortunately still a lot of work to be done. In the Netherlands, many people have yet to see the results of the “participation in employment” project. However, the factsheets have been very well received with a large amount of downloads occurring every month. These factsheets are now available in English. Johan believes that the success of the factsheets in the Netherlands demonstrates that they should be able to be translated into other languages and used in other counties.
The need for accessible, reliable, and universally understandable information remains crucial. He shared that according to recent findings, 26% of Dutch pharmacy visitors do not fully understand the purpose, instructions and potential side effects of the medications they receive.
This statistic underscores a growing disconnect between traditional communication methods and patient comprehension. “A quarter of our population is no longer connecting with the information we provide in the old way,” he remarked, emphasizing the urgency for change.
He acknowledged the need to perhaps explore innovative ways to deliver medical information, moving beyond traditional formats in order to ensure that every patient has access to the full story they deserve. “There is a serious problem,” he admitted, “and we must work harder, better, and differently to get the information across to everyone.”
We would like to thank Johan Beun for sharing his valuable perspective and expertise and hope you are more aware of the challenges faced by individuals with adrenal and pituitary disorders when it comes to employment. To explore this topic further, feel free to take a look at the resources below.
Additional resources
Websites:
- AdrenalNET (Dutch only)
- eu (multiple languages)
- online (Dutch only – work information for people with a chronic condition)
Employment Factsheets
- Cushing’s syndrome FACTSHEET
- Pituitary disorders FACTSHEET
- Adrenal Insufficiency FACTSHEET (in translation at this moment)
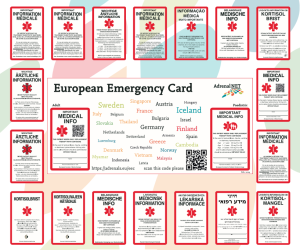
European Emergency cards:
Adrenal insufficiency Stress instructions:
- Guidelines on taking hydrocortisone to prevent an Addison’s crisis (available in multiple languages)