Adult Growth Hormone Deficiency
What is Growth Hormone?
What is Growth Hormone?
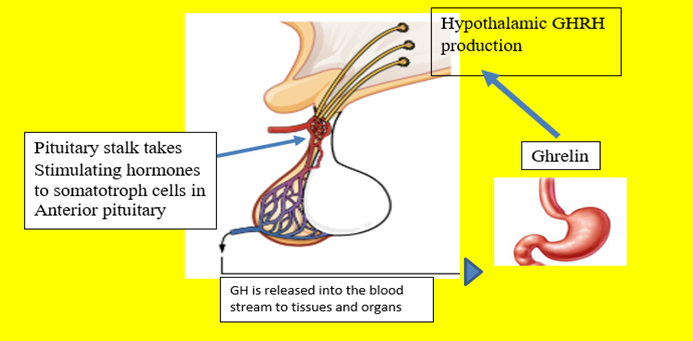
Growth hormone (GH) is known by several names, somatropin or human growth hormone (HGH). The production of GH is stimulated by growth hormone releasing hormone (GHRH) from the hypothalamus that travels down the pituitary stalk into the anterior pituitary, stimulating the production of Growth hormone (GH) in the somatotroph cells of the anterior pituitary. Other hormones such as Ghrelin from the stomach also stimulate GH production.
What does Growth Hormone do?
What does growth hormone do?
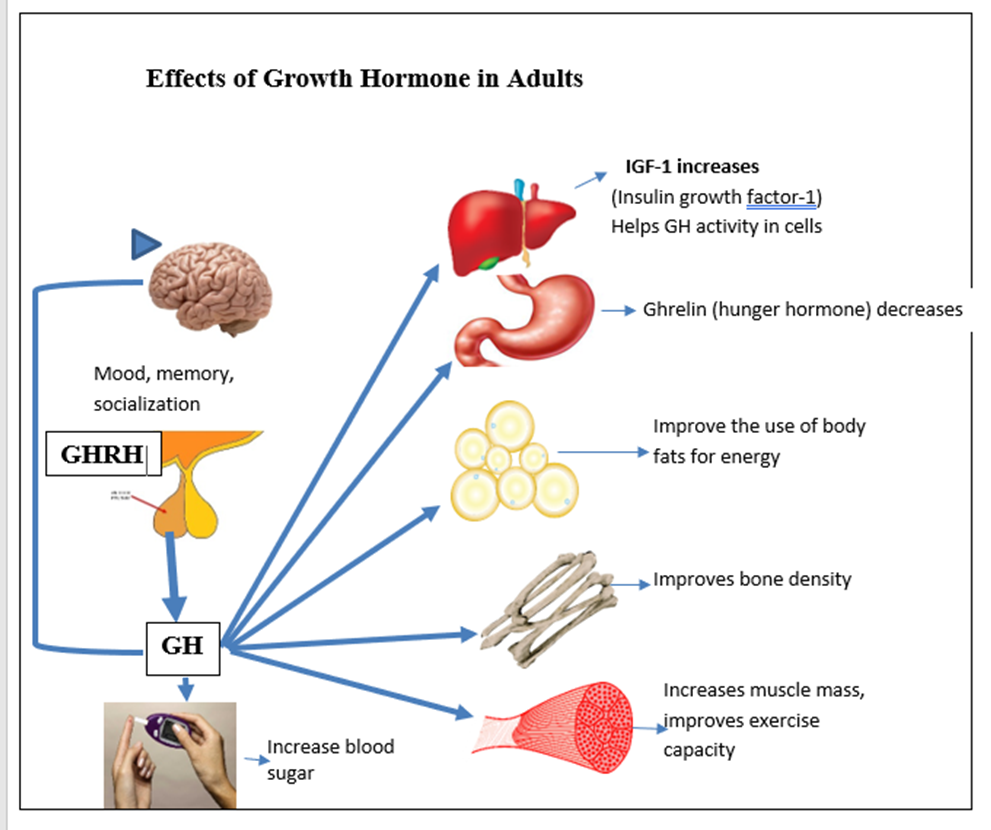
In childhood, GH is needed for growth of muscles, bones. It distributes and controls body fat and helps with glucose control.
In adulthood GH helps to decrease total body fat, improve muscle function, exercise capacity, energy, and decreases the risk of heart attacks and strokes. GH improves bone density and decreases the risk of bone fractures. Psychologic improvements in mood, interest in social activities and overall quality of life have been reported.
Note:
The total amount of growth hormone produced is different for men and women. The highest rates of growth hormone secretion occur during puberty, which is responsible for the adolescent growth spurt. Growth hormone level becomes lower as we grow older.
All pituitary functions are usually evaluated if growth hormone is suspected of being abnormal to help determine if other levels are affected.
What controls Growth Hormone (GH) secretion?
What controls growth hormone (GH) secretion?
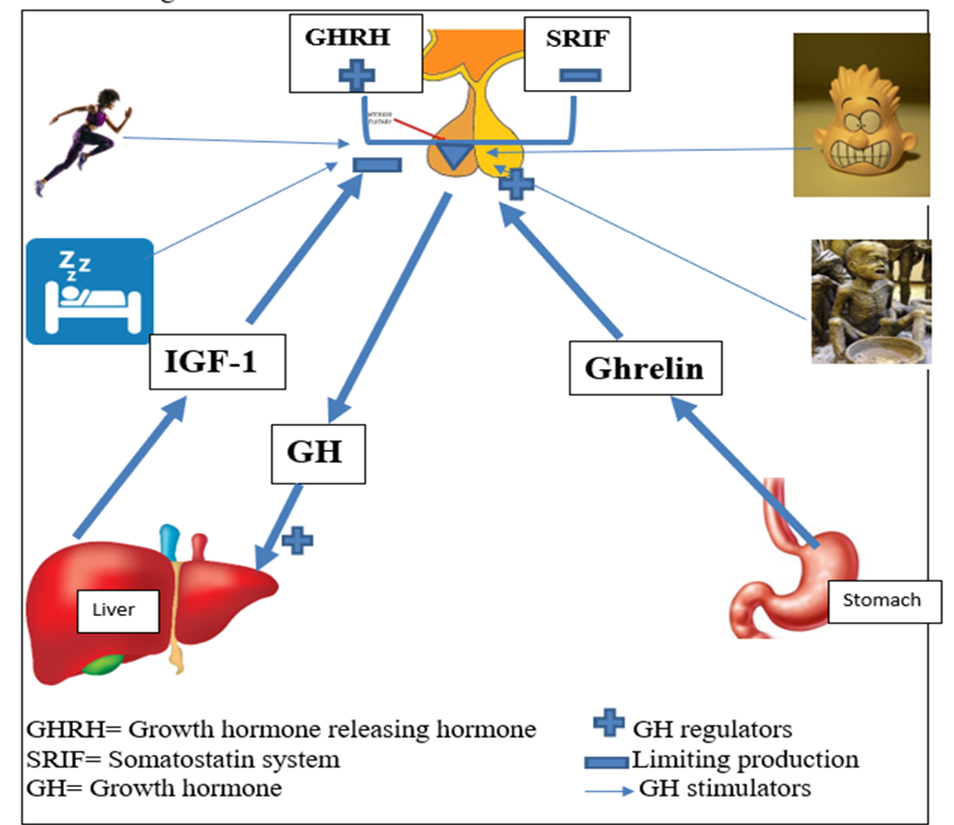
GH is released in irregular ‘pulses’ regulated by GHRH, somatostatin, IGF-1 and Ghrelin in a daily pattern. During fasting, or prior to meals, the hormone Ghrelin (GH releasing peptide) is released from the stomach signalling the hypothalamus to release GH releasing hormone (GHRH). This travels down the pituitary stalk instructing the somatotrophs of the anterior pituitary to make and release GH. GH attaches to multiple cells including on the liver where it makes insulin growth factor-1 (IGF-1). IGF-1does not have a daily rhythm of production but is used as a measure of GH activity. When the body senses enough IGF-1 a (negative) feedback message signals the hypothalamus and the pituitary to stop making and secreting GH.
During the day, GH stimulation occurs in response to hunger, a decrease in blood sugar, increased stress, and exercise. At night, shortly after the onset of sleep, the highest amounts are secreted for tissue growth and repair. GH circulates in the blood and is quickly absorbed into cells. Within 11-18 minutes after a ‘pulse’ of GH, blood levels are back to low baseline levels.
Somatostatin is a hypothalamic hormone that stops the production of GHRH to regulate the total amount of GH produced.
Effects of Adult Growth Hormone Deficiency (GHD)
Effects of Adult Growth hormone Deficiency (GHD)
Adult GHD is associated with increased body fat, midsection weight gain and high cholesterol levels. This increases the risk of strokes and heart attacks. Muscle and strength is lost and it is difficult to increase muscle with exercise. Energy and tolerance for exercise is low with easy fatigue. Bones may become brittle, have poor mineral density with a higher risk of bone fractures. High blood sugar is more likely because insulin is less effective at moving sugars into cells for use as energy. Cognitive function can also decline with decreased attention, and poor long term and working memory. GHD appears to decrease social interaction, sexual interest and affect other emotions.
Causes of Growth Hormone Deficiency in Adults
Causes of Growth Hormone Deficiency in Adults
The most common cause is a pituitary adenoma, after pituitary surgery or bleeding into the pituitary (apoplexy). However, radiation therapy to the brain and impacting the pituitary such as in treatment for brain cancers can also cause GHD. GHD can be the result of traumatic brain injury (TBI), subarachnoid haemorrhage or a severe disruption of blood supply to the pituitary such as in injury or severe blood loss. GHD may also persists from childhood. Obesity is also known to decrease GH production.
Diagnosis and Testing for Adult GHD
Diagnosis and Testing for Adult GHD
Growth hormone secretion is pulsatile making spikes and low levels difficult to catch with a random blood draw. A stimulated test is used for accuracy with specific diagnostic cutpoints for positive tests recommended by professional endocrine societies. Testing is usually not needed in adults with more than 3 pituitary hormonal deficiencies and a low IGF-1.
An insulin tolerance test (ITT) is the ‘gold standard’ of testing but not considered safe for use in persons with heart disease, epilepsy, or over 55 years. Insulin is administered to induce hypoglycaemia and stimulates GH production. Blood is drawn frequently to monitor sugar levels. Other tests include intramuscular injection of glucagon or an oral macimorelin stimulating test. Samples of blood for GH are taken prior to the any medication and GH levels are measured every 30 minutes for at least 90 minutes.
How is Adult GHD treated?
How is Adult GHD Treated ?
Current treatment is a daily subcutaneous injection of recombinant or manufactured growth hormone. Longer acting formulas are being evaluated but questions remain regarding tolerability and safety.
Several daily formulations of GH are now available. GH is usually self- administered from a pen style injector. A cartridge is inserted containing either liquid or powdered (lyophilized). In powder form, a liquid is infused into the powder when the pen and ‘primed’. A fresh, short, thin (small gauge) needle is attached daily and discarded after use. The patient dials the pen to the prescribed dose prior to injection. Injection sites can be selected on the abdomen or thighs and daily site rotation is recommended.
For women taking oestrogen, it is usually recommended to use transdermal preparations for best effect of the growth hormone.
A low dose may be prescribed initially and increased every 1-2 months to keep blood levels of IGF-1 in the mid-range of normal. Once stable IGF-1 levels have been achieved, blood IGF-1 level is monitored every 6 months.
Abbreviations
Abbreviations
GH Growth hormone
GHRH Growth Hormone Releasing Hormone
SRIF Somatostatin
GHD Growth Hormone Deficiency
ITT Insulin Tolerance Test
IGF-1 Insulin Growth Factor–1
References
References
Mark E. Molitch, David R. Clemmons, Saul Malozowski, George R. Merriam, Mary Lee Vance, Evaluation and Treatment of Adult Growth Hormone Deficiency: An Endocrine Society Clinical Practice Guideline, The Journal of Clinical Endocrinology & Metabolism, Volume 96, Issue 6, 1 June 2011, Pages 1587–1609, https://doi.org/10.1210/jc.2011-0179
Tritos NA, Biller BMK. Current concepts of the diagnosis of adult growth hormone deficiency. Rev Endocr Metab Disord. 2021 Mar;22(1):109-116. doi: 10.1007/s11154-020-09594-1. Epub 2020 Sep 22. PMID: 32959175.
Díez JJ, Sangiao-Alvarellos S, Cordido F. Treatment with Growth Hormone for Adults with Growth Hormone Deficiency Syndrome: Benefits and Risks. Int J Mol Sci. 2018 Mar 17;19(3):893. doi: 10.3390/ijms19030893. PMID: 29562611; PMCID: PMC5877754.
Jørgensen JO, Müller J, Møller J, Wolthers T, Vahl N, Juul A, Skakkebaek NE, Christiansen JS. Adult growth hormone deficiency. Horm Res. 1994;42(4-5):235-41. doi: 10.1159/000184199. PMID: 7868079.
Yuen KCJ, Biller BMK, Radovick S, Carmichael JD, Jasim S, Pantalone KM, Hoffman AR. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Growth Hormone Deficiency In Adults and Patients Transitioning from Pediatric to Adult Care. Endocr Pract. 2019 Nov;25(11):1191-1232. doi: 10.4158/GL-2019-0405. PMID: 31760824.
Takahashi Y. The Role of Growth Hormone and Insulin-Like Growth Factor-I in the Liver. Int J Mol Sci. 2017;18(7):1447. Published 2017 Jul 5. doi:10.3390/ijms18071447
Ho, K. K. Y., & on behalf of the 2007 GH Deficiency Consensus Workshop Participants. (2007). Consensus guidelines for the diagnosis and treatment of adults with GH deficiency II: a statement of the GH Research Society in association with the European Society for Pediatric Endocrinology, Lawson Wilkins Society, European Society of Endocrinology, Japan Endocrine Society, and Endocrine Society of Australia, European Journal of Endocrinology, 157(6), 695-700. Retrieved Nov 26, 2022, from https://eje.bioscientifica.com/view/journals/eje/157/6/695.xml
Author:
Chris Yedinak DNP, FNP
Associate Professor
Oregon Health & Sciences University Portland. OR, USA
Updated: November 2022
