Prolactinoma
What is Prolactin
What is Prolactin
Pro – before Lac- Milk
Prolactin is a hormone secreted by the pituitary gland that acts with other hormones for breast development and lactation in pregnancy and childbirth.
A prolactinoma is a prolactin secreting pituitary adenoma that is formed when a mistake in cell multiplication results in a large mass of prolactin producing cells.
Why is Prolactin important?
Why is Prolactin Important?
Many important hormones are secreted from the anterior pituitary. One group of cells in the anterior pituitary are called lactotrophs which secrete prolactin that is released into the blood stream.
Although prolactin contributes to other body functions, it is essential for breast tissue development and lactation in women and sexual function in men. Too little prolactin in women may result in difficulty breast feeding after childbirth, whereas, too much results in infertility in both sexes.
The hypothalamus produces the hormones that control prolactin balance. Levels may fluctuate a little for women during the menstrual cycle but are significantly higher during pregnancy and lactation. Nipple and chest wall stimulation, stress, light and some odours can stimulate prolactin production. A suckling infant stimulates the mother to produce high amounts of prolactin. While breast feeding, prolactin levels remain elevated. After breast feeding, levels will return to a lower level. Levels will return to a baseline or basal level after about 2 weeks without breast feeding.
How is Prolactin Production Controlled?
How is Prolactin Production Controlled?
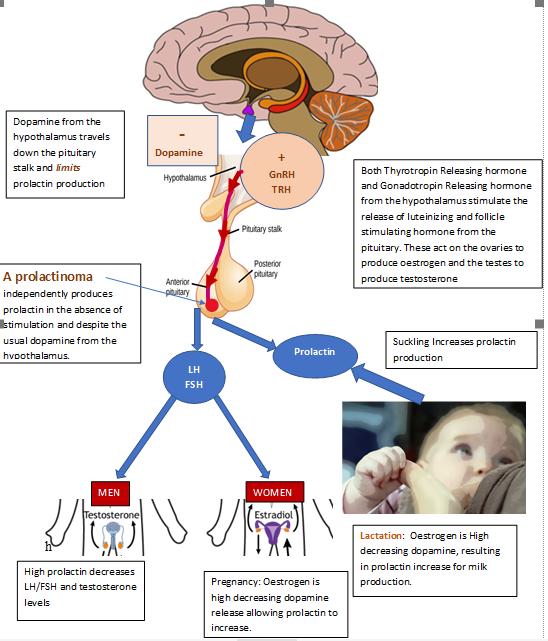
The hypothalamus controls the production and secretion of prolactin using a chemical substance called Dopamine. Dopamine is a chemical that is released from nerve cells in many parts of the brain including the hypothalamus. In a non-pregnant female, dopamine travels down the pituitary stalk from the hypothalamus instructing the lactotroph cells to limit the amount of prolactin produced. This is the opposite of other pituitary hormones that receive instructions from the hypothalamus to produce and released hormones from the anterior pituitary.
Other hypothalamic releasing hormones such as thyrotropin releasing hormone (TRH) and gonadotroph releasing hormone GnRH also control dopamine levels. TRH along with dopamine help to keep the level of prolactin stable. GnRH stimulates the production of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the anterior pituitary. LH and FSH stimulate the ovaries in women to make oestrogen and progesterone and the testes in men to make testosterone. Oestrogen levels in women increase and decrease with phases of the menstrual cycle. Oestrogen levels are high mid menstrual cycle and again toward the end of the cycle. If pregnancy does not occur at ovulation, oestrogen and progesterone levels fall.
During pregnancy and after childbirth there is a need for higher levels of prolactin to increase breast tissue and for breast feeding. Higher levels of oestrogen inhibit or decrease the production of dopamine allowing levels of prolactin to increase and women to lactate, particularly with suckling. Progesterone levels fall after delivery which also increases prolactin level. GnRH from the hypothalamus also decreases during breast feeding, signalling the ovaries to stop releasing eggs for fertilization, stopping the menstrual cycle and providing some protection against pregnancy.
In men, higher prolactin levels usually does not result in lactation but does decrease LH, FSH and testosterone levels resulting in infertility.
Likewise, several medications such as narcotics, tranquilizers, anti-nausea medications, birth control drugs and some antidepressants (serotonin uptake inhibitors) can decrease dopamine production and increase prolactin levels
Prolactin Production
Prolactin Production
Prolactinomas and Prolactin Excess
Prolactinomas and Prolactin Excess
A Prolactinoma is formed by abnormal multiplication of prolactin cells (lactotrophs) in the anterior pituitary due to a genetic mistake in cell replication. The cause of this ‘mutation’ is unknown. Prolactinomas are a benign (non-cancerous) tumour, often called an ‘adenoma’, that produce more prolactin than can be controlled by the regular mechanisms. Like most pituitary adenomas their growth is typically very slow over many years. Prolactinomas are the most common pituitary tumour and are more common in women than men.
In women, prolactinomas cause galactorrhoea, or lactation (milk production) when not pregnant or after an infant has been weaned and breast feeding has been stopped. Menstrual cycle becomes irregular or stops all together. Men rarely suffer from breast discharge but may experience breast enlargement (gynecomastia). Headaches and low interest in sex are common in both sexes with erectile dysfunction in men. Changes in body hair, acne and weight gain are also reported. If the tumour is large and presses on the nerves for the eyes that are located immediately above the pituitary gland, peripheral vision loss may occur in one or both eyes.
High prolactin inhibits gonadotropic releasing hormone (GnRH) secretion from the hypothalamus. Normally gonadotropin releasing hormone acts on cells in the anterior pituitary to make follicle stimulating hormone (FSH) and luteinizing hormone (LH). These hormones instruct female ovaries to make oestrogen and progesterone and male testes to make testosterone. However, high prolactin interrupts this signalling, resulting in the lack of a menstrual cycle in women (amenorrhea) and low testosterone (hypogonadism) in men and infertility.
In rare cases in young patients with rapidly growing tumours, a family history of pituitary tumours may be important to evaluate for an inherited form of prolactinoma. As previously noted, most prolactinomas are sporadic mutations or a spontaneous mishap of replication.
Prolactin and growth hormone have a common genetic ancestor and have similar chemical structures. Therefore, when prolactin is produced in excess from a pituitary tumour, growth hormone levels and symptoms of acromegaly are usually also evaluated.
Diagnosis
Diagnosis
The diagnosis of a prolactinoma is typically based on signs and symptoms and a blood test for an elevated prolactin level. A pregnancy test is also recommended at the same time as prolactin levels will be elevated in pregnancy. If the patient has no signs and symptoms but the prolactin is elevated, a test for ‘macroprolactin’ or an inactive form of prolactin will be drawn. Inactive forms of prolactin are not associated with any health issues. All pituitary hormone levels are usually assessed if an elevated prolactin is suspected.
Testing is done with a single blood draw which does not have to be done fasting or at any specific time of the day or part of the menstrual cycle. It is important to tell your endocrine team what medications you are taking particularly for birth control, nausea, depression, and high blood pressure. Avoid strenuous exercise, breast stimulation and extraordinary stress prior to this blood draw so that the test is accurate. In some cases, how the laboratory analyses the blood sample may also affect the results. Extremely high levels of prolactin from large tumours require the blood sample to be ‘diluted’ prior to analysis to ensure that the level is not falsely low.
A brain/pituitary MRI (magnetic resonance Image) is done to see if there is a pituitary tumour (adenoma), its size and how close it is to the optic chiasm or nerves leading from the eyes to the brain.
If vision is affected by a large tumour, visual field testing by an ophthalmologist or specialty eye doctor is usually recommended as part of an evaluation.
Treatment
Treatment
There are 3 main treatment options 1) medication to control prolactin production or 2) surgery to remove the tumour and 3) radiation.
Medications
Since dopamine inhibits prolactin release, medicine that increases dopamine called dopamine agonists (DA) are used. These increase the amount of dopamine released from the hypothalamus to stop prolactin release. Two DA medicines are available, bromocriptine and cabergoline. Although both drugs are effective at reducing prolactin levels and shrinking tumour, cabergoline may be used preferentially for its faster action to decrease prolactin levels and shrink prolactinomas.
Patients are cautioned to monitor for signs of medication intolerance and adverse reactions. In rare cases, cabergoline may shrink a tumour so rapidly that it causes a tear in the sac of cerebrospinal fluid around the brain. If this occurs the patient reports a severe headache and sticky, salty tasting liquid leaking from the nose and down the back of the throat. This requires urgent surgical correction, and the patient is referred to the nearest hospital emergency department. Other rare side effects may be depression and impulsive behaviours such as gambling, impulsive purchases or other ‘out of character’ behaviours. An echocardiogram may be recommended prior to starting cabergoline and during treatment to monitor for any changes in heart valves. Prolactin levels will be monitored frequently at first then every 6 to 12 months over time. Likewise, an MRI is usually done yearly at first and then less frequently if stable.
Medication may also restore fertility once prolactin level is lowered into the normal range, so if pregnancy is not desired, birth control is recommended. If the prolactin level has been normal for several years and there is no evidence of tumour on MRI, the medication may be stopped and both prolactin level and MRI monitored for a recurrence. Likewise, after menopause dopamine agonists may be stopped.
Surgery is usually only considered for individuals with large tumors, particularly if there is loss of vision, individuals who cannot tolerate medical therapy or if there is continued tumor growth despite medication. If the entire prolactinoma cannot be removed during surgery, or if prolactin levels remain elevated after surgery, medication may need to be continued after surgery.
Radiation
If prolactin level is not controlled after medical and surgical treatment, there is residual tumour or tumour growth, radiation therapy may be recommended. However, medication may still be needed until radiation therapy becomes effective.
Abbreviations
Abbreviations
PRL Prolactin
FSH Follicle Stimulating Hormone
LH Luteinizing hormone
MRI Magnetic Resonance Imaging
TRH Thyrotropin Releasing Hormone
GnRH Gonadotroph Releasing Hormone
DA Dopamine Agonists
References
References
Al-Chalabi M, Bass AN, Alsalman I. Physiology, Prolactin. [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507829/?report=classic
Cozzi, R., Ambrosio, M. R., Attanasio, R., Battista, C., Bozzao, A., Caputo, M., Ciccarelli, E., De Marinis, L., De Menis, E., Faustini Fustini, M., Grimaldi, F., Lania, A., Lasio, G., Logoluso, F., Losa, M., Maffei, P., Milani, D., Poggi, M., Zini, M., Katznelson, L., Luger, A., Poiana, C., & AME. (2022). Italian Association of Clinical Endocrinologists (AME) and International Chapter of Clinical Endocrinology (ICCE). Position statement for clinical practice: prolactin-secreting tumors, European Journal of Endocrinology, 186(3), P1-P33. Retrieved Nov 24, 2022, from https://eje.bioscientifica.com/view/journals/eje/186/3/EJE-21-0977.xml
Mancini T, Casanueva FF, Giustina A. Hyperprolactinemia and prolactinomas. Endocrinol Metab Clin North Am. 2008 Mar;37(1):67-99, viii. doi: 10.1016/j.ecl.2007.10.013. PMID: 18226731
Author:
Author: Chris Yedinak DNP, FNP
Associate Professor
Oregon Health & Sciences University Portland. OR. USA
Updated November 2022
