October is Pituitary Awareness month and while this month may be coming to an end, raising awareness for pituitary disorders remains as important as ever. In this WAPO Blog we will cover some of the reasons why raising awareness for pituitary disorders is something we should all striveto do.
Because the pituitary gland regulates many of our body’s functions
The pituitary gland, a small structure located under the hypothalamus of the brain, controls the functions of the hormone-secreting endocrine glands throughout the body. Due to this ability to regulate the hormones of the body that act on various organs, a dysfunction in the pituitary gland can lead to imbalances that affect many of our natural processes, including growth, metabolism, and reproduction. Our mood and emotions can also be affected. These hormonal imbalances can lead to irreversible changes in the body and comorbidities that can have a significant impact on a patient’s quality of life and life expectancy. It is therefore crucial to raise awareness for the pituitary gland and the role it plays in our overall health and for the conditions that can cause it to dysfunction.
Because their initial symptoms can be mistaken for more common conditions
Some of the presenting symptoms of pituitary disorders can be non-specific and mimic other more common conditions. Adrenal insufficiency, for example, may present with fatigue, weakness, nausea and weight loss, which can be falsely attributed to anxiety or gastrointestinal problems. Cushing’s syndrome may present with weight gain, hypertenstion and fatigue, which can easily be attributed to obesity.
This means that many patients with a pituitary disorder often visit numerous doctors before receiving a correct diagnosis. In a recently published meta-analysis of multiple studies, the average time from symptom onset to diagnosis in patients with pituitary-related Cushing’s syndrome was 38 months. However, some patients have reported waiting as long as 20 years before being diagnosed.
This indicates that there is an urgent need to raise awareness for pituitary disorders in the medical community so that general practitioners can recognize specific patterns of symptoms and unusual presentations that may indicate a pituitary disorder.
Educating the general public about some of the “red flags”of pituitary disorders can also prompt people to ask their doctor about these signs or symptoms, hopefully decreasing their time to diagnosis. For example, “red flags” for prolactinoma include absent or irregular periods associated with milk production from the breasts (unrelated to pregnancy) in girls and sexual dysfunction in males. Some “red flags” for acromegaly include an increase in shoe size or enlarged hands with rings no longer fitting. Raising awareness for pituitary disorders is one way to spread this kind of valuable knowledge.

To increase the chance of early diagnosis and prevent long-term complications
The earlier the diagnosis of a pituitary disorder, the better the outcome.
Patients with acromegaly, for example, can suffer from comorbidities affecting the cardiovascular, respiratory, metabolic, neuropsychiatric, and musculoskeletal systems. These comorbidities can impact both their quality of life and their life expectancy, if the increased production of growth hormone (GH) and insulin-like growth factor-1 (IGF-1) is left untreated. However, if diagnosed and treated early, these comorbidities can be prevented or delayed.
Various studies have shown that the mortality rate in people with acromegaly reverses to that of the general population if adequate treatment is provided to normalize GH and IGF-1 levels.
In people with adrenal insufficiency, which is characterized a lack of cortisol production from the adrenal glands, early diagnosis is key when it comes to ensuring better long-term outcomes for patients. Firstly, being diagnosed early can save patients from presenting with a life-threatening adrenal crisis. Secondly, it allows them to start hormone replacement therapy in order to correct the glucocorticoid deficiency and help alleviate their symptoms. Finally, with a diagnosis they can receive patient education on how to adapt their medication in times of stress or illness and learn the importance of carrying an emergency hydrocortisone kit with them at all times.
In order for this to take place there needs to be more actions to ensure that primary care providers are aware of these diseases so that patients can be quickly referred to an endocrinologist for a timely diagnosis.
To break loneliness and isolation
When diagnosed with a pituitary disorder many people describe a feeling of loneliness and isolation due to the rarity of their disease. Depending on the specific condition, it may be difficult to find anyone living with the same disease in your area. This is exactly what Claire Barlow and Jennifer Kenworthy experienced after being diagnosed with Sheehan’s syndrome (postpartum pituitary necrosis). That was until they decided to create Maternal Pituitary Support in order to provide support to other women and advocate for maternal pituitary disorders (listen to their story in the WAPO Vlog here).
Finding a patient organization that supports people living with either their specific condition or group of conditions is an important step in a patient’s journey. Even when properly supported by their friends and family, nothing replaces the feeling of someone truly understanding what you and your family are going through. Having a group of people with lived experience, that can guide you through the day to day challenges you may encounter, is so important. Caregivers can also benefit from meeting others that care for someone with a pituitary disorder.
By raising awareness for pituitary disorders and the associated patient organizations, there is a better chance that patients and caregivers will find others like themselves and locate the right support groups that can improve their mental health and overall quality of life.
To empower patients to self-advocate
When we see others like ourselves in advocacy roles, we are more likely to want to join in, learn more about our condition, and share our stories. This is why the participation of patient advocates in awareness raising activities is so important. Patient advocates that share their experience of living with a pituitary disorder give others the courage to equally share their voice, creating a ripple effect of advocacy actions and empowerment.
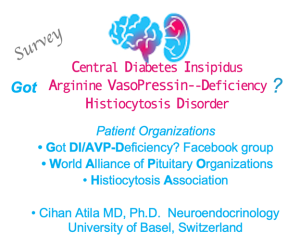
Never underestimate the power that your story can have on someone else! This is why WAPO strives to share patient stories, such as in its WAPO Vlogs Cushing Syndrome Comorbidities: Priorities for Patients Vs Healthcare or Shining Light on Arginine Vasopressin Deficiency (AVP-D)/ Central Diabetes Insipidus.

To increase awareness around invisible disabilities
Like many rare diseases, pituitary disorders are often accompanied by invisible disabilities including fatigue, pain, sleep disturbances, and mental health disorders such as depression and anxiety.
Patients report that these invisible disabilities can have a significant impact on their quality of life. Lack of understanding from family members, co-workers or the general public can lead to feelings of isolation. Relationships can become strained if there is a lack of empathy or misunderstanding from people thinking that the patient should be “back to normal” after receiving treatment.
This is similar for patients with any chronic disease that carries an invisible disability, which is why taking the time to understand the invisible disabilities experienced by patients with a pituitary disorder can help you be more aware of this term and more compassionate towards others who share their invisible disabilities with you in the future. To learn more about invisible disabilities, you can visit the Hidden Disabilities website.
To increase access to specialized care
Because pituitary conditions have a huge impact on the body and multiple organ systems, it is important that they are treated by a multidisciplinary team with expertise in managing endocrine disorders. However, in some countries, no reference centers with expertise in pituitary disorders exist. Advocacy efforts led by patients gave rise to the creation of the European Reference Networks for Rare Diseases, and of ENDO-ERN (the ERN for Rare Endocrine Conditions) in particular, in 2017. Within this network, the healthcare provider members have all been recognized as reference centers for endocrine conditions and they can provide virtual consultations, through a dedicated platform, to doctors with patients in countries all across Europe. This allows for geographical inequalities, in terms of access to specialized care, to be decreased.
By raising awareness for pituitary disorders with healthcare professionals and policy makers, we can ensure that funding is provided to support and develop initiatives that allow patients to receive the treatment they need, no matter where they live.

Now that you have a list of reasons why raising awareness for pituitary disorders is so important, why not help us share information and advocate for the people living with these conditions.
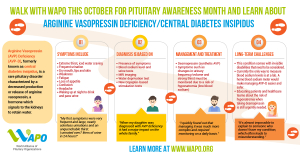
You can start by sharing the four “Walk with WAPO” posters we created this year for Pituitary Awareness Month on Arginine-Vasopressin Deficiency, Cushing’s Disease, Adrenal Insufficiency and Acromegaly (download them here).
You can also make sure to follow WAPO on our social media channels so that you can share our posts with your network. Learn more about the many pituitary disorders on the WAPO website so that you can recognize their symptoms and educate those around you.
Together we can help to make the future brighter for all people living with a pituitary disorder!
References:
Rubinstein, German et al. “Time to Diagnosis in Cushing’s Syndrome: A Meta-Analysis Based on 5367 Patients.” The Journal of clinical endocrinology and metabolism vol. 105,3 (2020): dgz136. doi:10.1210/clinem/dgz136
Norman, Alyson et al. “Hidden disability: a study of the psychosocial impact of living with pituitary conditions.” British journal of nursing (Mark Allen Publishing) vol. 31,11 (2022): 590-597. doi:10.12968/bjon.2022.31.11.590
Brue, Thierry, and Frederic Castinetti. “The risks of overlooking the diagnosis of secreting pituitary adenomas.” Orphanet journal of rare diseases vol. 11,1 135. 6 Oct. 2016, doi:10.1186/s13023-016-0516-x
Gadelha, Mônica R et al. “Systemic Complications of Acromegaly and the Impact of the Current Treatment Landscape: An Update.” Endocrine reviews vol. 40,1 (2019): 268-332. doi:10.1210/er.2018-00115
Bleicken, Benjamin et al. “Delayed diagnosis of adrenal insufficiency is common: a cross-sectional study in 216 patients.” The American journal of the medical sciences vol. 339,6 (2010): 525-31. doi:10.1097/MAJ.0b013e3181db6b7a